A 35yr old female elog.
A case of a diabetic with breathlessness
Note:
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome.
(Under the guidance of Dr. Sai charan sir PG, and Dr.G. Kusuma ma'am intern)
Patient was admitted to the hospital in the afternoon of 28th June,2021.
"Chief complaints"
- Fever and Diarrhea since 5 days( 4 to 5 times a day with blood discharge).
- Back pain( 5 days ago) with abdominal pain and chest pain.
"History"(as told by the patient's daughter because she was unconscious at the time)
- The pt. was diagnosed with Type 2 Diabetes 3 years ago and was put on some oral hypoglycemic agents along with Mixtard injection( 20U-x-14U) (currently on medication)
- The pt. had visited the hospital regularly for evaluation after she was diagnosed with the condition.She had also followed the diet prescribed by a fellow medical practioner.
- 2 years ago she developed an infection in the little finger as it couldn't be treated,the infected area was removed.
- Back pain had occured 1 year ago for which she took antibiotics( without any prescription) which worsened the pain.
- Before visiting the OPD, she complained of severe breathlessness and pain in the chest region.
- Her GRBS(general random blood sugar) was 580mg/dl for which 10 units of insulin was infused.
COURSE In hospital with intubation and CPR notes :
35 F/1/0 DM: 4 yrs on " H. MIXTARD S/c PD
(2014)
c/o fever,pain in abdomen.. Altered Sensorium(1day) vomiting, loose stools( 4 days )
Pt came to casualty @ 1:00 pm on 28/6/21 in a state of altered sensorium.
INTUBATION & CPR -
At 1:40 pm Patient Suddenly became unresponsive (Gasping)
No recordable PR
BP-NR
SPO2 -60% MRA
ABG showed severe M. Acidosis.
CPR was initiated Acc. to 2015 AHA guidelines & intubated I ET 7.0
ROSC obtained after 3 cycles of CPR & Connected to mechanical ventilator
ACMV mode
VT: 420 ml
FiO2 : 60%
RR: 14 cpm
Bp 80/50mmHg
PR -110 b/m
SPO2 98%
CVS - s1, s2 heard.
RS -BAE bilateral air entry
NVBS heard
Per Abdomen: Soft and tender
Family history :
Not significant.
Medical history :
- A diabetic alone, not a known case of hypertension,asthma or tuberculosis.
- She hasn't undergone any surgery in the past.
Drug history :
- She was on treatment for diabetes.
- Not a smoker or an alcoholic.Not a drug addict .
"General examination"
- Pallor :present(palpebral conjunctiva)
- Icterus:absent
- Cyanosis:absent
- Clubbing of extremities: absent.
- Oedema:absent
- Lymphadenopathy:absent
- Patient was initially conscious on arrival. Later she had become unconscious.
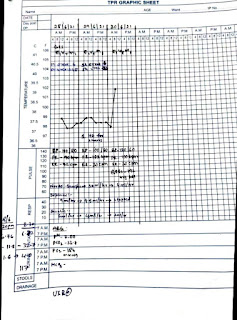
Vitals:
- BP :Initially her BP was fluctuating between 80/50 and 90/40. Later she was put on Noradrenaline infusion after which her BP was stagnant at 110/90.
- RR : 36 Cycles/min.
- Pulse:86beats/min.
- Temperature : Afebrile.
Respiratory system examination :
- Normal vesicular breath sounds.
- No crackles
- No wheezing heard.
- No chest wall deformity.
Cvs examination :
- S1 S2 heard.
- No thrills.
- Cardiac murmurs absent.
Abdominal examination :
- Soft
- Non tender
- No palpable masses
Cns examination :
- Unconscious / altered
- Speech no response
- No signs of meningeal irritation
- GCS (coma scale) :E 3 V 4 M 5 ( before arrest )
- After arrest E 1 V T M1
- Yesterday also same GCS
- Today E1 V T M4
Provisional diagnosis: DKA with AKI ( ? Pre renal)
USG(25/06/21) - Pyelonephritis.
Laboratory investigations :
ABG analysis:Day 1
Day 2)
ABG analysis
Liver function tests:
Day 3

Day 4
Day 5
Post dialysis reports
Day 6 and 7
Bed soresBP 150/80mmHg
PR 89c/m
Ventilator was disconnected
SpO2 98% on oxygen mask.
GCS E4 V1 M4
No change in treatment.
Spleen-normal
Rt. Kidney - 9x4.5cm N S/E, CMD(+), PCS(N)
IMPRESSION :
Left Kidney 13.2x7.5cm increased size, abnormal echogenicity of раrenchyma noted with Ћуро and hyper echoic regions.
However no E/O air focii was noted. However no e/o any abscess, Perinephric collections, mild hydronephrosis in left PCS
Aorta I.V.C. - (N)
No Ascitis
No lymph-adenopathy
U.bladder - normal Empty
V-U Junctions - Foley'sbulb insitu.
Uterus-Size - Pelvis couldn't be assessed
Parenchyma with (Lt)Abnormal echogenicity, mild hydronephris ,no perinephric collections suggested
clinical corelation to
Acute pyelonephritis
.
Day 8 - An MRI scan was done
Complete debriment upto muscle was done.
Patient is still in a persistent vegetative state.
No prognosis is seen.
Have started treating her with antibiotics.
Also physiotherapy was suggested but there is no improvement in her state.
Treatment :
Day 1
Inj. NORAD 2amp in 50ml NS
Inj. PIPTAZ 2.25gm.
Inj. DOPAMINE 2amp in 50ml
Inj. HAI 1ml in 39ml NS
Day 2
Inj.HAI 1ml in 39mlNS
Inj. PIPTAZ 2.25gm.
Inj. CLEXANE 40gm.
Iv infusion NS RL @100ml/hr.
Day 3
Inj.HAI 1ml + 34ml NS
Inj. PIPTAZ 2.25gm
Iv infusion NS (urine output + 40ml/hr)
Inj. NORADRENALINE(2 amp+46ml NS)
Day 4,5 same as day 3
Day 6
Inj. PIPTAZ
Inj. LEVOFLOX
Inj. VANCOMYCIN
Day 7 and 8 same as day 6.
Day 9
Inj. MEROPENEM
Inj. LEVOFLOX
Inj.VANCOMYCIN
Day 10 and 11 same as day 9
Day 12
Inj. MEROPENEM
Inj. FOSFOMYCIN
Inj. CLEXANE
Day 13 and day 14 same treatment as of day 12 additionally Inj. LASIX was given.
Discharge summary :
Expected date of discharge :
Diagnosis :
Chief complaints :
- Fever and Diarrhea since 5 days( 4 to 5 times a day with blood discharge).
- Back pain( 5 days ago) with abdominal pain and chest pain.
"History"(as told by the patient's daughter because she was unconscious at the time)
- The pt. was diagnosed with Type 2 Diabetes 3 years ago and was put on some oral hypoglycemic agents along with Mixtard injection( 20U-x-14U) (currently on medication)
- The pt. had visited the hospital regularly for evaluation after she was diagnosed with the condition.She had also followed the diet prescribed by a fellow medical practioner.
- 2 years ago she developed an infection in the little finger as it couldn't be treated,the infected area was removed.
- Back pain had occured 1 year ago for which she took antibiotics( without any prescription) which worsened the pain.
- Before visiting the OPD, she complained of severe breathlessness and pain in the chest region.
- Her GRBS(general random blood sugar) was 580mg/dl for which 10 units of insulin was infused.
Family history :
Not significant.
Medical history :
- A diabetic alone, not a known case of hypertension,asthma or tuberculosis.
- She hasn't undergone any surgery in the past.
Drug history :
- She was on treatment for diabetes.
- Not a smoker or an alcoholic.Not a drug addict .
"General examination"
- Pallor :present(palpebral conjunctiva)
- Icterus:absent
- Cyanosis:absent
- Clubbing of extremities: absent.
- Oedema:absent
- Lymphadenopathy:absent
- Patient was initially conscious on arrival. Later she had become unconscious.
Vitals:
- BP :Initially her BP was fluctuating between 80/50 and 90/40. Later she was put on Noradrenaline infusion after which her BP was stagnant at 110/90.
- RR : 36 Cycles/min.
- Pulse:86beats/min.
- Temperature : Afebrile.
Respiratory system examination :
- Normal vesicular breath sounds.
- No crackles
- No wheezing heard.
- No chest wall deformity.
Cvs examination :
- S1 S2 heard.
- No thrills.
- Cardiac murmurs absent.
Abdominal examination :
- Soft
- Non tender
- No palpable masses
Cns examination :
- Unconscious / altered
- Speech no response
- No signs of meningeal irritation
- GCS (coma scale) :E 3 V 4 M 5 ( before arrest )
- After arrest E 1 V T M1
- Yesterday also same GCS
- Today E1 V T M4
Provisional diagnosis: DKA with AKI ( ? Pre renal)
Treatment :
Inj. NORAD 2amp in 50ml NS
Inj. PIPTAZ 2.25gm.
Inj. DOPAMINE 2amp in 50ml
Inj. HAI 1ml in 39ml NS
Day 2
Inj.HAI 1ml in 39mlNS
Inj. PIPTAZ 2.25gm.
Inj. CLEXANE 40gm.
Iv infusion NS RL @100ml/hr.
Day 3
Inj.HAI 1ml + 34ml NS
Inj. PIPTAZ 2.25gm
Iv infusion NS (urine output + 40ml/hr)
Inj. NORADRENALINE(2 amp+46ml NS)
Day 4,5 same as day 3
Day 6
Inj. PIPTAZ
Inj. LEVOFLOX
Inj. VANCOMYCIN
Day 7 and 8 same as day 6.
Day 9
Inj. MEROPENEM
Inj. LEVOFLOX
Inj.VANCOMYCIN
Day 10 and 11 same as day 9
Day 12
Inj. MEROPENEM
Inj. FOSFOMYCIN
Inj. CLEXANE
Day 13 and day 14 same treatment as of day 12 additionally Inj. LASIX was given.










































Comments
Post a Comment